
The Science Behind Pilates and Osteoporosis: How Pilates can Support Bone Health
Osteoporosis is a condition characterised by a loss of bone density, making bones brittle and more susceptible to fractures. Osteopenia, often a precursor to osteoporosis, indicates lower-than-normal bone density without reaching the severity of osteoporosis. With an ageing global population, the number of people affected by these conditions is on the rise, highlighting the need for proactive measures in maintaining and improving bone health. For Pilates teachers, understanding the science behind osteoporosis and how Pilates can play a key role in supporting bone health is crucial for effectively working with this population.
Understanding Bone Physiology
To comprehend how Pilates supports bone health, we must first understand the basics of bone physiology. Bones are living tissues, continuously undergoing a process of remodelling, where old bone is broken down (resorption) and new bone is formed (formation). This balance between resorption and formation is essential for maintaining bone strength and density.
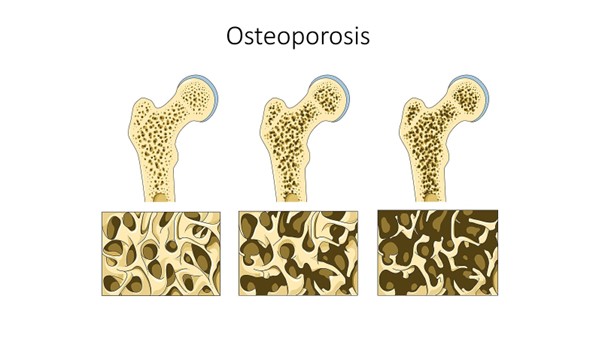
From left to right, normal bone, Osteopenia and Osteoporotic bone
(Image credit: Wikimedia commons: Meyers Konversations-Lexikon, 4th edition (1885–1890))
In individuals with osteoporosis or osteopenia, the rate of bone resorption exceeds the rate of bone formation, leading to a net loss of bone density. Factors such as age, hormonal changes (especially in post-menopausal women), lack of physical activity, and inadequate nutrition can all contribute to this imbalance.
The Role of Exercise in Bone Health
One of the most effective ways to combat bone loss is through weight-bearing exercise. Weight-bearing exercises, such as walking, dancing, and resistance training, place mechanical stress on the bones. This stress stimulates bone remodelling by signalling the osteoblasts (bone-forming cells) to build new bone tissue, thereby strengthening the bones.
Pilates, traditionally known for its focus on core strength, mobility, and posture, can also provide these weight-bearing benefits. This means we need to take our client up out of supine and get them working against gravity to stimulate bone density while at the same time improving posture and balance. With careful modifications, Pilates can be an invaluable tool for clients with osteoporosis and osteopenia, helping to improve bone density, posture, balance, and overall strength, all while reducing the risk of fractures.
How Pilates Supports Bone Health
Pilates exercises can be particularly beneficial for clients with osteoporosis or osteopenia in several ways:
- Weight-Bearing and Resistance Exercises
Weight-bearing exercises, in which the body works against gravity, are a key component in improving bone density. Pilates offers many standing exercises and those that involve the use of springs and resistance bands, such as the Standing Leg and Arm Springs on the Cadillac, which apply effective load to the bones. Additionally, using equipment like the Wunda Chair or Reformer allows clients to perform resistance exercises, targeting specific muscles and bones. The resistance provided by springs and body weight challenges the bones to respond to site specific exercises that have applied progressive overload strategies. Instead of choosing footwork on the Reformer, do this seated on the Wunda Chair. Do lunges on the chair. Do scooter and standing side splits on the Reformer.
- Improved Balance and Coordination
A major concern for clients with osteoporosis is the increased risk of falls, which can lead to fractures, especially in vulnerable areas like the hips, spine, and wrists. Pilates helps improve balance and coordination, reducing the likelihood of falls. Exercises like Standing Leg Press on the Chair or Standing Side Splits on the Reformer and standing arm springs with the Cadillac engage the stabilizing muscles around the hips, legs, and core, promoting better stability and proprioception.

- Spinal Alignment and Postural Support
One of the primary dangers of osteoporosis is vertebral fractures, often caused by excessive forward bending or poor posture. Many individuals with osteoporosis may experience an excessive forward curvature of the spine (kyphosis) because of vertebral wedge shaped compression fractures.
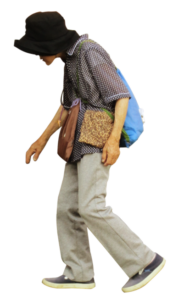
An osteoporotic elderly woman in Japan. Her increased Kyphosis is due to wedge shaped compression fractures in her thoracic spine.
(Image credit: Wikimedia creative commons. 7 October 2011)
Pilates emphasises postural alignment, teaching clients to lengthen the spine, open the chest, and engage the deep core muscles.
By strengthening the muscles around the spine and teaching clients how to maintain proper alignment, Pilates can help reduce the risk of spinal fractures. Exercises like regressed Swan on the Mat or Reformer, which focus on spinal extension, are beneficial in counteracting kyphosis and promoting a more upright posture. When doing these exercises place a pillow under the abdomen to protect the ribs.

- Building Core Strength for Spinal Support
A strong core is essential for supporting the spine and reducing the risk of fractures. In Pilates, many exercises are designed to engage the deep abdominal muscles, pelvic floor, and lower back muscles, collectively known as the core. For clients with osteoporosis, building core strength can help protect the spine from excessive compression and support better movement patterns.
For instance, exercises like Pelvic Curls or Bridging on the Mat or Reformer help strengthen the core. When doing these exercises opt for a straight back without spinal flexion promoting safe movement of the spine. We must modify exercises to avoid excessive spinal flexion, which could increase the risk of fractures in osteoporotic clients. So, eliminate exercises such as abdominal curls, washer woman on the chair, Monkey on the Cadillac.
Modifications and Safety Considerations
When working with clients who have osteoporosis or osteopenia, it’s essential to modify exercises to ensure safety. Certain movements, such as high-impact exercises, deep spinal flexion (e.g., rolling like a ball), and extreme spinal rotation, should be avoided, as they can increase the risk of fractures. Instead, we should focus on exercises that emphasize gentle spinal extension, axial elongation, and weight-bearing movements that are within the client’s capacity.
We should also pay close attention to the client’s individual needs and health history. Some clients may have specific areas of weakness or past fractures that require additional modifications. Communication with healthcare providers, including doctors and physical therapists, is crucial to ensure that the Pilates program complements any medical treatments or restrictions. Ask your clients for a copy of their most recent DEXA scan report. Ask them for copies of any X-ray reports. I was surprised when I received an x-ray report from a new client that she had compression fractures in her spine. This made it very clear to me to guide her away from the spinal flexion exercises she was doing at home that she presumed was keeping her spine supple.
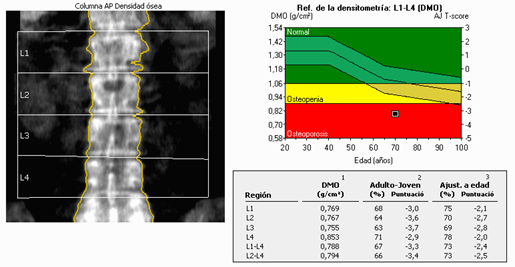
Bone density is measured with a DEXA scan or Dual-Energy X-ray Absorptiometry. This is a Dual-Energy X-ray Absorptiometry image of lumbar vertebral column with osteoporosis. Woman 70 years old. You can see in the report the black square is in the red section which is classified as Osteoporosis. It looks like her T-score is a – 3.
(Image credit: Wikimedia creative commons.)
Educate clients how to move on and off the equipment so as not to flex through the spine. They can then use this information to help them when getting in and out of bed. Also how to sit softly in a chair rather than plonking down. When someone with osteoporosis sits hard down into a chair this is direct spinal loading and can cause spinal fracture if their Osteoporosis is severe. Teach clients sit-to-stand exercises with a focus on sitting slowly, get them to incorporate this into their day, so that whenever they sit it is with a slow and controlled movement, building their bone density at the same time and warding off future fractures.

Please see this link for some ideas on how to work in the Pilates studio to move safely and to build bone. https://youtu.be/f0Sle9iswFo?si=NVSdUp6R8toPm7E3
Pilates can be an effective tool in supporting clients with osteoporosis and osteopenia, offering benefits such as improved bone health, enhanced balance, better posture, and core strength. However, it’s important to have a solid understanding of the condition and make appropriate modifications to exercises to ensure safety and efficacy. By integrating weight-bearing and resistance exercises into Pilates sessions and focusing on spinal alignment and balance, Pilates teachers can help their clients maintain and even improve bone health while reducing the risk of fractures.
As awareness of osteoporosis grows, we have a unique opportunity to provide specialised care that promotes long-term health and well-being.
Louise Taube
Member Special Offer
Pilates for Osteoporosis and Osteopenia online course with Louise Taube is PAA approved for 15 PDPs
Louise is offering PAA members 25% off the course using code BUILDBONE25 enrol here
About Louise Taube
Louise Taube is a renowned Pilates teacher trainer with a deep passion for helping others improve their physical health and well-being through Pilates. With over two decades of experience in the industry, Louise has become a sought-after expert in Pilates education, particularly in training instructors to teach specialized populations, including those with osteoporosis and osteopenia. She is known for her holistic approach, blending traditional Pilates techniques with modern science to create safe and effective programs tailored to individual needs. Louise’s dedication to her craft and her ability to inspire both students and fellow instructors have made her a respected leader in the Pilates community.
References
Anatomy & Physiology, Connexions Web site. http://cnx.org/content/col11496/1.6/, Jun 19, 2013.
BruceBlaus Blausen.com staff (2014). “Medical gallery of Blausen Medical 2014”. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/osteoporosis
https://www.healthdirect.gov.au/osteoporosis
https://www.healthline.com/health/osteoporosis
https://www.mayoclinic.org/diseases-conditions/osteoporosis/symptoms-causes/syc-20351968
https://www.medicalnewstoday.com/articles/155646
https://www.osteoporosis.foundation/
OpenStax College. Anatomy & Physiology, Connexions Web site. http://cnx.org/content/col11496/1.6/, Jun 19, 2013.
Melioguide https://melioguide.com/
Meyers Konversations-Lexikon, 4th edition (1885–1890)

Comments are closed.