Arthritis in a Pilates Studio
Reprinted with kind permission of Body Organics. Link to original article (including videos): A Spring in Your Joint
When we hear the term “arthritis” it can be a little confusing as people will say they have arthritis but there are over 100 types of arthritis. Each type of arthritis can play out in many different systems of the body so will not all present the same. As Pilates teachers it is likely that you will have many clients with some of these different types of arthritis.
In this article we will look at the group of arthritis conditions, the categorisations and some simple strategies for working with clients with “arthritis”.
What is Arthritis?
Arthritis is a term describing a condition in which there is inflammation of joints. In this article we will look at:
- the more common types of arthritis which have been categorised to help better understand their impacts of joints and other conditions.
- some commonalities in the medication treatments of these various arthritis, and we will discuss this later in the article
- principles of some appropriate exercises and modifications.
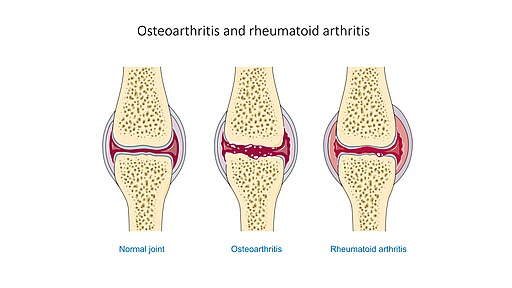
When we consider the inflammation of a joint we need to understand what the type of connective tissue is around the joint that is inflamed. The various types of arthritis could affect connective tissue such as:
- Chondral cartilage (Osteoarthritis)
- Synovium (Rheumatoid arthritis)
- Tendons (Psoriatic arthritis)
- Skin (Scleroderma)
The inflammation and changes in the connective tissue will have different pulls on the joint which can lead to deformities affecting its function.
What are the common types of arthritis?
There are many types of arthritis and the categories you are most likely to see in your studios are discussed below.
Osteoarthritis (OA) – This is the degenerative arthritis you are likely to see in older people. It can occur in younger people as well in joints that have been affected by trauma or injuries. It is where the chondro cartilage around the joints has been worn away and there is no longer protection around the joint ends of the bones. It is important to remember that the subchondral bone, periosteum, periarticular ligaments, periarticular muscle spasm, synovium and joint capsule are all richly innervated and are the source of nociception in OA (Hunter, McDougall, Keefe.2008) In other words it is believed that the loss of cartilage between the joints exposes the pain receptors and this is what prompts the reported pain when they are irritated.
A strategy for these clients is to ensure that you protect the joints from further wear and tear to the cartilage when working with them in the studio. The joints most commonly affected are the knees and specific joints in the hand.
Rheumatoid Arthritis (RA) is an auto-immune inflammatory disorder that typically affects the joints of the hands, feet and spine. However, it can also affect the neck, jaw and even the sterno-clavicular joint. Whilst it may occur in one joint area, it may not affect other joints. The joints affected can sometimes appear quite random, but the pattern is generally symmetrical. Visceral organs and eyes can also be affected.
The chronic inflammation that is a consequence of the condition contributes to joint swelling, stiffness, and pain in the synovial membrane of the joint capsule. The synovial lining essentially creates the fluid that helps the joints to slide on each other – it is like the oil that is used in machines to stop friction. When this fluid is reduced, friction can damage the chondral cartilage of the bones from the outside of the bone inwards, due to constant wear and tear. This is important as there are important pain receptors in the outer layer of the bone, and this is part of the pain experienced by those affected by RA. In the later stages, fibrosis (hardening of the soft tissue like scarring) of the joint capsule occurs. Cysts and bone spurs can also form around the joint, contributing to pain and stiffness. All of this can affect the bone and cartilage, thus impacting the movement quality the joint can achieve.
There are genetic predispositions to RA and it can run in families. You must have the gene in order for development, but the expression of the gene into the condition is not automatic. Geneally, there is some event that triggers the gene and the development of RA.
As with many autoimmune conditions, you are more likely to have RA if you are a woman. RA has been noted to develop after women have had their first child, with the reason for this being unknown but hormonal changes are suspected. It is also important to note that Rheumatoid Arthritis is one of those autoimmune conditions that can relate to other diseases (known as co-morbidity) and this includes Diabetes Type 1. There are also other complications from the condition including Sjorgren’s syndrome, depression and lung problems. People with RA have a two to four times higher risk of developing non-Hodgkin’s lymphoma than those without. Other blood cancers, such as leukemia and other forms of lymphoma, as well as lung cancer and melanoma, are also at a higher risk of occurring in those with RA. Not only is the disease itself a culprit, but some associated medications may be involved.
Spondyloarthritic diseases – Some more well known examples of this type of arthritis are Ankylosing Spondylitis (AS) and Psoriatic Arthritis (PA). These types are associated with damage to the neck, spine and sacrum. A follow up blog and material will be provided on these conditions.
Infectious Arthritis is a result of an infection from bacteria, virus, parasite or fungi. You may already be seeing some of this in your clients post a CoVid 19 infection. This kind of arthritis is often accompanied by a fever and chills. If treated quickly there will most likely be little damage, and treating the infection is an important element. One of the considerations is that if the infection can triggers other infections or long term inflammation as you see in conditions such as long covid, fibromyalgia and so forth.
Reiter’s syndrome or Reactive Arthritis occurs when an infection in one part of your body triggers immune system dysfunction and inflammation in a joint elsewhere in your body. The infections are generally in the gastrointestinal tract, bladder, or sexual organs. If treated quickly the reaction should only last about 12 months. However, there can be issues with damage to the joint affected from this arthritis that can eventually lead to osteoarthritis.
Systemic lupus erythematosus (SLE) is another autoimmune disease that can affect your joints and connective tissue in your body.
Fibromyalgia syndrome, a condition in which your brain processes pain in your muscles and joints in a way that amplifies your perception of the pain. This is such a huge topic it really needs to be considered in a separate blog.
Scleroderma, an autoimmune condition in which inflammation and hardening in your skin connective tissues can lead to organ damage and joint pain.
Medications
When we talk about these various arthritis you will note that many have similar medications and treatments as the medications are targeting reduction in inflammation and specific immune pathways. The common treatments include:
- Steroids to reduce the inflammatory response
- Immune suppressing medications eg methotrexate
- Immunotherapies such as biologics
As always it is important to check with your client about their medications and any side effects. Sometimes, you need to spend more time focussing on the side effects of these medications than the actual disease. This is particularly common in some of the autoimmune related arthritis where clients will be taking immune suppression medications. Some of the considerations include:
- Long term steroid use can result in bone density issues eg osteopenia and osteoporosis
- Peripheral neuropathies
- Light sensitivities
- Memory and cognitive impacts
- Fatigue
- Reflux
There are many more possible symptoms, so remember to stop and check with the clients about the various conditions.
Movement principles
When working through these conditions it is important to remember that our focus is not on some false argument that exercise and movement is a cure. Rather our focus is:
- Maintaining function – Helping the person find ways to continue to use their affected limbs. This could involve working with an occupational therapist to have splints made for the joint which are then used whilst the person is doing specific exercises. – Teaching compensatory techniques such as strengthening and working proximally, so that the person reduces the load on the distal joints.
- Protect the joint – Ensure that we work to maintain congruency (alignment) of the joints to reduce the likelihood of deformities – Modifications and specific muscle strategies in repertoire choice. – Remembering that some of these arthritis are intermittent and that after a “flare” the person will still have some damage to the joint and will need ongoing protection.
- Manage fatigue and inflammatory responses.
- Manage your studio environment – eg reduce glare as many types of arthritis affect light sensitivity, manage safety.
For more specific information about the various types of arthritis you can contact PAA level 4 Professional Instructor Carla Mullins at Body Organics Education, as she has a vast resource of knowledge and material about this topic. In 2023 she will be releasing a course called Springing this Joint which is focusing on arthritic conditions.
References
Hunter DJ, McDougall JJ, Keefe FJ. The symptoms of osteoarthritis and the genesis of pain. Rheum Dis Clin North Am. 2008 Aug;34(3):623-43. doi: 10.1016/j.rdc.2008.05.004. PMID: 18687276; PMCID: PMC2597216.
Comments are closed.