
Guest article by Ash Berry, PAA L1 Member
Link to original: Is Deep Breathing Always the Answer?
Late last year I attended a two day BreatheAbility breathing course with physiotherapist and Breathing Educator Tess Graham. Tess Graham trained with Ukrainian doctor Konstantin Buteyko in the early 1990’s. Buteyko is renowned for his work on breathing retraining for asthmatics and founding the Buteyko Institute. Tess herself has over 6500 hours of clinical experience as a breathing specialist and believes she cured two of her children of their asthma. Naturally, being curious and a Pilates instructor, I was eager to learn about her techniques for breathing retaining which, until now, I hadn’t heard of.
We take for granted our ability to breathe
Breathing is the most important thing for us to survive, and all systems of the body are at least linked and perhaps even dependent on our breathing. Yet because it happens automatically, we don’t usually focus on it and when we do, it’s often because we are instructed to take deep breaths. Deep breathing has been used for decades to encourage us to calm ourselves down or settle into a relaxed state in a yoga, Pilates or meditation class. However, the BreatheAbility Level 1 course looks at deep breathing as an encouragement to over-breathe, a common dysfunctional breathing pattern observed in many of us. In fact, analysis of minute volume measurements of “healthy normal” people over the last 20 years indicate that up to 90% of the population over-breathe chronically. (Reference: T.Graham 2018 of Rakhimov A.) So instead of deep breathing, Tess focuses on retaining and practising what is physiological normal breathing for humans in terms of exchanging of gases, blood chemistry and brain oxygenation.
What is physiological normal breathing?
Physiological normal breathing is measured by 8-12 breaths per minute in your average adult. Breaths are regular, smooth and gentle. Breathing occurs in and out through the nose, which facilitates diaphragmatic breath and overall breathing should be silent and almost invisible.
Signs of over-breathing are mouth breathing or audible breathing, irregular sighs, yawns or coughs, snoring, sleep apnoea, asthma and anxiety. Tess has concluded that 80% of adults with anxiety disorders are chronic mouth breathers, forming a correlation between over-breathing and anxiety.
It can be difficult to measure this without a hospital grade spirometer or a sleep study, however people can self-test by counting their breaths over one minute, checking their heart rate over one minute and subjectively analyse themselves breathing throughout the day. For example: Do you catch yourself with your mouth open often? This would be a sign of over-breathing.
Why is this so important?
Our lungs have the capacity to hold 4-6 litres of air at any one time. From the moment a baby takes their first breath, there is a residual volume kept in the lungs, that helps keep the alveoli (air sacs in the lungs) from collapsing (see at base of graph). This means we have approximately 3-5 litres of voluntary lung capacity also known as vital capacity. Despite this, our lungs have a tidal volume (that is the amount of air that moves in and out of the lungs for breathing at rest) of only 500ml or approximate 10% of our lung capacity. So at rest we only want to breathe approximately 10% of our total vital capacity. This ultimately means if we are taking deep breaths we are likely moving into our inspiratory and expiratory reserve volumes. This can be necessary for certain types of breathing, eg: hypopressives, Pranayama breath, etc and we refer to this as ‘special effects breathing’, however for the regular everyday exchange of gases, 500ml or 10% is considered physiological normal breathing.
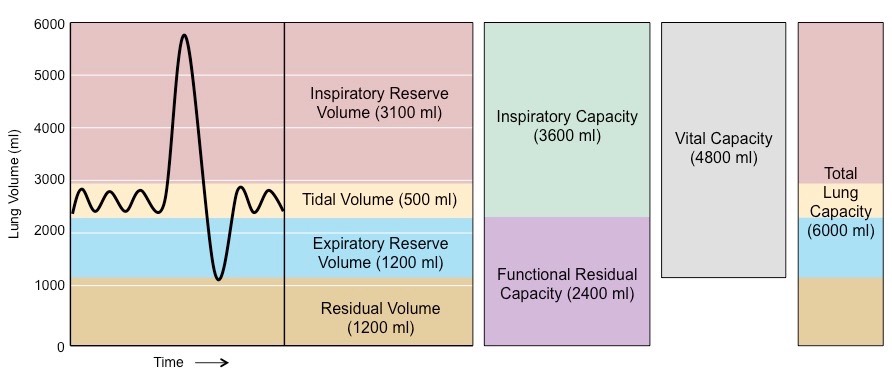
http://ib.bioninja.com.au/standard-level/topic-6-human-physiology/64-gas-exchange/lung-capacity.html
CO2 is not the enemy
Breathing allows for the exchange of gases, inhaling oxygen (O2) and exhaling carbon dioxide (CO2) which in turn allows the blood to be oxygenated to keep us alive. However here is the catch. We’ve often been taught that CO2 is a waste gas that needs to be expelled from the body, but in fact our bodies need CO2 to ensure oxygenation of the blood. (The Bohr Effect) Tess describes it as CO2 being the bus driver and all the O2 molecules sitting on the bus. It doesn’t actually matter how much O2 is on the bus when it enters the body, if the CO2 (bus driver) isn’t there to open the door of the bus, the O2 can’t be released into the blood. So the CO2 facilitates blood oxygenation and therefore brain and body oxygenation.
CO2 has a number of other positive characteristics as well. It is a natural buffering system for our bodies, helping to regulate many systems. It is a natural bronchodilator, antihistamine, sedative and muscle relaxant. It promotes digestion by relaxing the smooth muscle of the gut and plays an important role in balancing and regulating pH balance.
CO2 also stabilises our mast cells. Mast cells occur in places like our gut wall and our sinuses/ nasal pathways. Our mast cells are responsible for releasing histamine when faced with combating inflammation or allergic reactions. CO2 can act as a natural defense mechanism for problems with chronic inflammation eg: leaky gut, sinusitis, allergies or at the more serious end of the scale some autoimmune conditions, by stabilising our mast cells, making our immune system more resilient. Among many other benefits, CO2 helps with getting us off to sleep, keeping us asleep and down-regulating our nervous system so we are not always operating in ‘fight or flight’.
The differences between Pilates breath and physiological normal breathing
With all this great new information I started to analyse how it relates to what we teach in Pilates. Joseph Pilates took what he knew from many movement modalities including gymnastics, yoga and martial arts, all which have certain ‘special effects’ breathing techniques. Pilates too has its own versions of ‘special effects’ breathing – just think about the Hundred! Pilates breath can also be taught in different ways depending on the teacher. Below I made a table of the similarities and differences between Pilates breath and what is considered physiologically normal.

Copyright Movementality 2019
Things to practice?
Awareness is the first step
Start to notice how you breathe throughout the day; can you hear yourself breathe? Where do you initiate your breath from? Also check in to see if your preference is nasal or mouth breathing and if you catch yourself with your mouth open. You may be surprised! At the start of the course I recorded my expected nasal breathing being at about 80% given it’s something I’ve been mildly aware of the last 12 months. When I started to become more acutely aware, I changed my answer to 20%.
Check in with your posture
(If you do Pilates, this will be second nature to you.) Posture wants to be upright but not tense. Tess encourages her clients to imagine a coat hanger in the place of their shoulders and their body hanging off the coat hanger. In my classes I talk about an ‘internal lift’, subtle from the outside and even between the front and back body. Good posture facilitates diaphragmatic breathing.
Reduce your cloud
Imagine you have a cloud above your body that represents that amount of air you breathe in with each breath. Imagine the council is going to now charge you for that air, so you’re going to try to reduce the volume of air you intake by breathing less. Try to breathe 1-5% less air over the next 7 days. Don’t try to change things too rapidly either. By being aware, there will be changes anyway, and remember if at any point you feel uncomfortable, you are trying to change too much too fast. Take it slow!

Somatic Workshop with breath awareness. Copyright Movementality 2018
The Cross Examination
The thing I liked most about Tess’s workshop is that it was heavily rooted in human physiology and science based, so it makes a lot of sense. Despite that she has struggled to receive any funding for research to back up her work and the Buteyko Method is still not considered by the Australian Government Department of Health as an alternative therapy that can be covered by health insurance. Another interesting thing to note is that modern textbooks have slightly upped the rate of breaths per minute for the average adult to 12-16. Tess addressed this figure, comparing it to clothing brands upping their sizes to accommodate an obesity crisis. She believes modern day stress has contributed to this ‘average’ breath rate increase but questions the benefit of raising the stats to make over-breathing appear more normal. I did some digging into the proposed benefits of deep breathing to see how the stats compare. In most cases, deep breathing was okay but forced deep breathing was not because it can upset your body’s natural balance. Although I am very intrigued and eager to delve deeper into Tess Graham’s theories regarding breathing and have felt positive impacts in applying this to myself, the takeaway message for me at this stage is that breathing is highly subjective and it is important to allow others to breathe in a way that feels comfortable to them, whether that be a little gentler or a little deeper and refrain from ‘choreographed’ or ‘counted’ breathing that may challenge their physical norm.
If you are interested in learning more about physiological normal breathing, I’d recommend checking out Tess Graham’s two books, Relief from Snoring and Sleep Apnoea (Penguin,2012) and Relief from Anxiety and Panic by changing how you breathe (2017) both available via her website.
Comments are closed.